Basal Body Temperature: 7 Proven Ways It Boosts Fertility
The phrase “basal body temperature” (BBT) refers to the body’s minimum resting temperature, one that is often taken as soon as one wakes, a short whereas subsequent to any physical progress having occurred. There are other physiological changes, especially those occurring during the menstrual cycle, that influence this temperature, which reflects the metabolic condition of the body. As BBT affects the region of early pregnancy and is an important indicator of ovulation, knowing it is pertinent to pursuing regenerative flourishing.
Measuring BBT requires a dependable thermometer and a reliable schedule. Ladies are energized to take their BBT at the same time each day, beneath comparable resting conditions, to guarantee exactness. A advanced thermometer particularly planned for BBT estimation is regularly suggested, as it gives exact readings. Recordings can be archived on a chart or an app, permitting for less demanding design acknowledgment over time.
The pertinence of BBT in regenerative wellbeing lies in its capacity to show hormonal changes inside the body. Taking after ovulation, a woman’s progesterone levels rise, coming about in a slight increment in BBT, regularly approximately 0.5 to 1 degree Fahrenheit. This rise can be supported for a few days and regularly implies that ovulation has happened. For those attempting to conceive, following BBT can upgrade the understanding of ripe windows, empowering more educated choices approximately the timing of intercourse.
Additionally, observing BBT can give bits of knowledge into early pregnancy. A supported rise in temperature past the normal premenstrual stage may propose that conception has taken put, demonstrating potential pregnancy. In this setting, BBT rises as a pivotal device for ladies energetic to get it their regenerative cycles and back their family arranging endeavors. By reliably following basal body temperature, people can develop more prominent mindfulness of their ripeness designs and by and large regenerative health.
1.How Basal Body Temperature Fluctuates
Basal body temperature (BBT) is characterized as the most reduced body temperature watched amid rest periods, regularly measured promptly upon waking. All through the menstrual cycle, BBT encounters eminent vacillations administered by hormonal changes, fundamentally estrogen and progesterone. Understanding these shifts is basic for those following ovulation and early pregnancy signs.
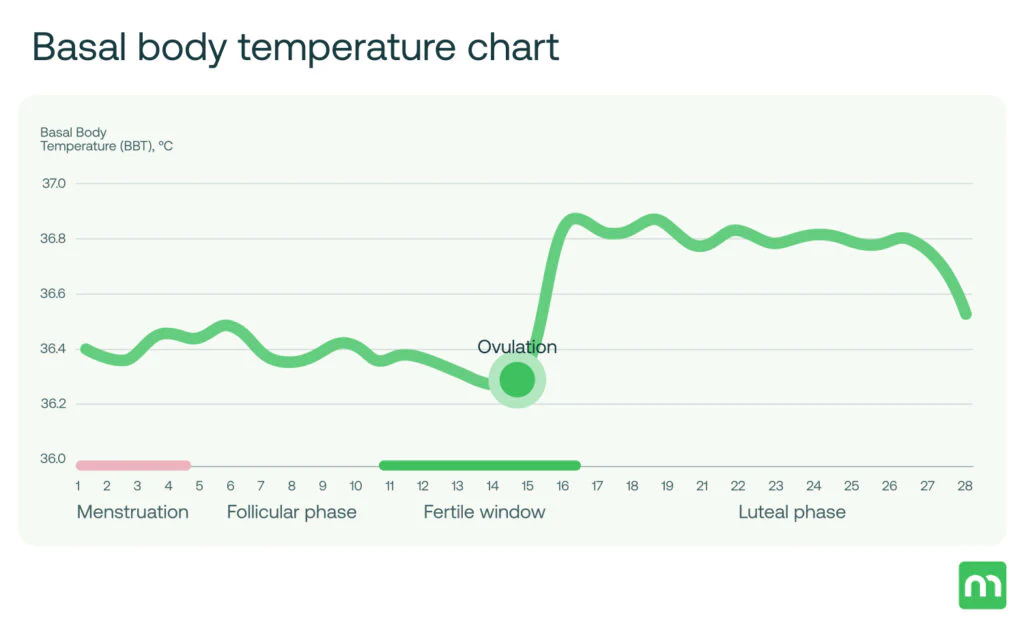
During the follicular stage of the menstrual cycle, which begins on the to begin with day of feminine cycle and proceeds until ovulation, estrogen levels rise slowly. This hormonal surge leads to a slight diminish in BBT or stabilization of temperature levels, for the most part watched between days 1 to 14 of the cycle. Variables such as rest quality and ailment can too change BBT amid this time; in any case, these varieties are regularly negligible compared to those seen in afterward phases.
As ovulation approaches, estrogen crests, activating a surge in luteinizing hormone (LH), which in turn leads to ovulation. This occasion more often than not happens around day 14 of a ordinary cycle. Taking after ovulation, the cracked follicle changes into the corpus luteum, which secretes progesterone. It is this hormone that altogether raises BBT, frequently by 0.5 to 1.0 degrees Fahrenheit (or 0.3 to 0.6 degrees Celsius). The lifted temperature remains until the onset of menstruation.
In the luteal stage, which endures from ovulation until feminine cycle, the nearness of progesterone is vital. If fertilization of the egg happens, progesterone levels proceed to rise, keeping up a higher BBT to bolster a potential pregnancy. Alternately, if fertilization does not happen, progesterone levels drop, driving to a return to pattern temperatures and the onset of feminine cycle. Observing these hormonal variances can offer profitable bits of knowledge for ladies interested in understanding their ripeness windows and conceivable early pregnancy indicators.
2.BBT Charting: Strategies and Best Practices
Charting basal body temperature (BBT) is a profitable procedure for those attempting to conceive, as it makes a difference identify ovulation and can flag early pregnancy. To start, it is fundamental to select the right strategy for measuring BBT, as exactness is foremost. The most common apparatuses incorporate advanced thermometers, which give fast readings, and basal thermometers, outlined particularly for identifying slight changes in body temperature. A basal thermometer is ordinarily more exact, permitting for the discovery of temperature shifts as negligible as one-tenth of a degree.
The timing of temperature estimation plays a pivotal part in the viability of BBT charting. In a perfect world, BBT ought to be taken instantly after waking, some time recently getting out of bed or locks in in any physical action. This hone guarantees that outside variables, such as development or nourishment admissions, do not impact the temperature perusing. Consistency in the time of estimation is foremost; subsequently, pointing to take the temperature at the same time each morning is fitting. For those taking after sporadic plans, keeping the thermometer following to the bed can help in recollecting to take the estimation upon waking.
In expansion to steady timing, it is vital to utilize a orderly approach to recording temperatures. Make a BBT chart, either carefully or on paper, to track day by day readings. Numerous people discover it accommodating to incorporate extra perceptions, such as menstrual stream, cervical bodily fluid changes, or other ripeness signs. This comprehensive approach permits for way better recognizable proof of designs over time. Moreover, keep up consistency by following to comparative rest conditions; disturbances, such as rest hardship or sickness, can influence BBT readings.
By taking after these strategies and best hones, people can viably chart their BBT, improving their capacity to recognize ovulation and screen regenerative wellbeing precisely. This fastidious consideration to detail can altogether progress the chances of conception and give important bits of knowledge into one’s menstrual cycle.
3.Identifying Ovulation Through BBT Tracking
Basal Body Temperature (BBT) following serves as an important apparatus for those looking for to get it their menstrual cycle, especially in connection to ovulation. This strategy rotates around measuring the body’s resting temperature, which can move due to hormonal changes all through the menstrual cycle. Ordinarily, BBT remains moderately moo amid the follicular stage driving up to ovulation, and at that point a discernible increment happens after ovulation has transpired.
The rise in BBT ordinarily falls inside the extend of 0.5 to 1.0 degrees Fahrenheit, this rise is fundamentally credited to progesterone surge after the discharge of an egg. To viably track ovulation, it is fundamental for people to take their temperature each morning at the same time, some time recently any physical action or utilization of nourishment, guaranteeing reliable readings. The amassed information over a few cycles can be plotted on a chart, uncovering designs that are significant for recognizing the ovulation window.
When translating BBT charts, the unmistakable temperature increment signals that ovulation has likely happened, stamping the conclusion of the prolific window. Prolific days are characterized by the days driving up to this temperature move. Recognizing this design not as it were helps in timing intercut but too improves the chances of conception. Couples pointing to conceive ought to in a perfect world lock in in sexual intercut in the days driving up to the rise in temperature, as sperm can live in the female regenerative tract for a few days, maximizing the probability of fertilization.
Incorporating BBT following into one’s schedule cultivates a way better understanding of person cycles and regenerative wellbeing. This strategy engages people to take charge of their ripeness, permitting for educated choices with respect to conception or indeed family arranging. Extra components, such as stretch and sickness, may affect temperature readings, hence it is imperative to consider these components when analyzing ovulation designs from BBT charts.
4.The Association Between BBT and Early Pregnancy
Basal Body Temperature (BBT) serves as a critical marker for ladies endeavoring to get it their regenerative wellbeing, especially in identifying ovulation and the early signs of pregnancy. Following BBT includes measuring the body temperature upon waking, which can vary all through the menstrual cycle. Amid the luteal stage, post-ovulation, it is common for BBT to rise somewhat due to expanded progesterone generation. This temperature rise by and large continues until feminine cycle happens if the egg is not fertilized.
In the setting of early pregnancy, a supported height in BBT is frequently one of the pointers that conception may have happened. After implantation, which more often than not happens almost six to ten days post-ovulation, progesterone levels stay lifted, driving to a continuation of raised BBT. For ladies who fastidiously chart their temperatures, taking note a maintained rise of 0.5°F or more over their ordinary pre-ovulation standard can flag early pregnancy. In any case, it is pivotal to note that whereas an hoisted BBT can recommend pregnancy, it is not authoritative verification, as different variables can impact body temperature.
Additionally, early pregnancy may go with other physical side effects, counting missed periods, weakness, and changes in breast delicacy, which together with BBT following can give a more comprehensive picture. Hence, ladies ought to combine BBT checking with other strategies, like domestic pregnancy tests or meetings with healthcare suppliers, for more exact evaluations. Understanding the relationship between drawn out lifted BBT patterns and the plausibility of pregnancy helps in upgrading information approximately one’s regenerative wellbeing. Through these perceptions, ladies can way better explore their choices with respect to family arranging and wellbeing management.
5.Common Misguided judgments Almost BBT and Fertility
Basal Body Temperature (BBT) observing is regularly encompassed by different myths that can lead to errors with respect to its part in richness. One common misinterpretation is that a rise in BBT ensures effective ovulation. Whereas an increment in temperature can demonstrate that ovulation has happened, it does not guarantee that an egg is practical for fertilization. The discovery of a temperature move is only one portion of the ovulation prepare, and numerous extra variables can influence richness, such as hormonal levels and generally regenerative health.
Another predominant myth is that BBT following is an trustworthy strategy for foreseeing ovulation. In reality, basal body temperature can be impacted by various outside variables, counting sickness, rest designs, and indeed push. These factors can lead to mistakes in temperature readings, making it imperative for people attempting to conceive to consider BBT as one of a few devices in their richness toolkit, or maybe than a standalone solution.
Additionally, a few individuals accept that BBT following is as it were significant for ladies attempting to conceive. Be that as it may, understanding BBT can moreover be advantageous for those looking to maintain a strategic distance from pregnancy. By recognizing the designs related with ovulation, people can lock in in more educated family arranging hones. Besides, there is a misguided judgment that BBT following is excessively complex. Whereas it does require commitment, the prepare can be direct and is encouraged by different apps and devices outlined to offer assistance clients record and translate their information effectively.
Addressing and debunking these misguided judgments is fundamental for those exploring richness ventures and can lead to a more educated and engaged approach to regenerative wellbeing. Picking up a clearer understanding of BBT and its suggestions can enormously improve one’s capacity to make educated choices with respect to ripeness and family planning.
6.Factors Influencing BBT Readings
Basal body temperature (BBT) is a imperative pointer in understanding regenerative wellbeing, especially in recognizing ovulation and early pregnancy. Be that as it may, a few outside and inside components can altogether impact BBT readings, requiring a comprehensive understanding for precise information elucidation.
One conspicuous inside calculate is ailment. The body’s reaction to diseases or sicknesses can result in raised temperatures as the resistant framework works to combat pathogens. This increment in temperature can darken the characteristic BBT design, possibly deceiving those attempting to track their ovulation cycle. Moreover, hormonal vacillations related with menstrual cycles, push, and other physiological changes can too contribute to varieties in BBT.
Lifestyle choices play a vital part in influencing BBT readings. For occasion, liquor utilization can raise body temperature incidentally and disturb ordinary BBT designs. Additionally, conflicting rest designs and shifting rest length can affect readings, as BBT ought to in a perfect world be measured after a least of three hours of nonstop rest for exactness. Disturbances, such as late-night shifts or visit travel, can lead to critical irregularities in recorded data.
Medications, particularly those influencing hormonal levels, such as hormonal contraceptives or ripeness drugs, can too have a significant affect on BBT. These medicines may misleadingly hoist or lower temperature readings, clouding women’s understanding of their normal ovulation cycles. Besides, natural changes, such as regular temperature changes, discuss conditioning, or warming frameworks, can influence an individual’s basal temperature. All these variables emphasize the significance of following BBT reliably, whereas considering outside impacts that may skew elucidations. By recognizing these fluctuations, people can make more educated choices around their regenerative wellbeing.
7.BBT Devices and Innovation: Cutting edge Solutions
Tracking basal body temperature (BBT) has gotten to be progressively available much appreciated to headways in innovation. With a plenty of devices accessible, people pointing to identify ovulation and screen early pregnancy can discover arrangements that fit their way of life. The most commonly utilized gadget for measuring BBT is a advanced thermometer, which offers improved precision and fast readings compared to conventional glass thermometers. Numerous advanced thermometers are particularly planned for ripeness following, highlighting touchy estimation scales that can identify indeed slight temperature shifts significant for deciding ovulation.
Furthermore, numerous present day thermometers come prepared with highlights that permit for simpler information logging. A few gadgets adjust with applications on smartphones, naturally recording temperature readings and giving visual representations of BBT patterns over time. These applications not as it were spare time but moreover minimize the chances of human blunder amid manual section. In expansion to following temperature, such apps frequently consolidate other richness pointers, such as cervical bodily fluid consistency and cycle length, giving a comprehensive see of one’s regenerative health.
Furthermore, wearables such as smartwatches and wellness trackers have presented another layer of comfort. A few of these gadgets can persistently screen body temperature and other physiological measurements, empowering clients to get real-time experiences almost their richness cycles. By combining BBT estimations with heart rate and rest designs, these devices can improve the precision of ovulation expectations, advertising clients a wealthier understanding of their cycles.
As people consider which devices to utilize, it is fundamental to reflect upon individual inclinations, from the want for real-time information to the ease of integration with existing innovation. Eventually, selecting the right BBT following instruments can enable people on their travel toward identifying ovulation and early pregnancy effectively.
Conclusion
The hone of following your Basal Body Temperature is a foundational procedure in regenerative wellbeing, giving a one of a kind window into the complex hormonal move of the menstrual cycle. Your Basal Body Temperature alludes particularly to your body’s temperature at total rest, which is why it must be measured instantly upon waking, some time recently any physical action, talking, or indeed sitting up, as these can cause slight rises that cloud the unpretentious, pivotal data.
The center rule is that a woman’s Basal Body Temperature is affected altogether by the hormone progesterone. In the to begin with half of the cycle (the follicular stage), Basal Body Temperature readings tend to be lower. Be that as it may, after the ovary discharges an egg (a prepare called ovulation), the coming about structure, the corpus luteum, starts emitting progesterone. This hormone has a thermogenic impact, causing a particular and supported shift—typically a rise of 0.5 to 1 degree Fahrenheit—in your Basal Body Temperature. This move is so solid that a supported height in your Basal Body Temperature for at slightest three sequential days is considered a essential biomarker for affirming that ovulation has in fact taken place.
For people and couples attempting to conceive, this makes the fastidious charting of Basal Body Temperature an important instrument. By watching this warm move, they can recognize that the ripe window has fair passed, which makes a difference them arrange for ensuing cycles with more noteworthy exactness. Moreover, if fertilization and implantation happen, the proceeded generation of progesterone implies the Basal Body Temperature will stay lifted, making a tirelessly tall Basal Body Temperature past the luteal stage one of the most punctual distinguishable signs of pregnancy.
The utility of checking your Basal Body Temperature expands distant past conception. It serves as a effective, low-cost demonstrative instrument for generally gynecological and hormonal wellbeing. A chart that appears whimsical temperatures, a disappointment to see a clear biphasic design (a moo stage taken after by a tall stage), or a brief tall stage can give clues almost conditions such as anovulatory cycles (where no egg is discharged), luteal stage absconds, or thyroid issues. Hence, a long-term record of your Basal Body Temperature offers a personalized report card on cycle normality and hormonal balance.
Historically, this was done with uncommon thermometers and paper charts, but innovation has revolutionized the handle. Various computerized apps and keen thermometers are presently outlined particularly to track, record, and analyze Basal Body Temperature, making the handle more open and precise by consequently charting the information and making a difference to recognize the move. This long-term examination of Basal Body Temperature charts uncovers designs that are one of a kind to each person, advertising profoundly personalized bits of knowledge that nonexclusive cycle following cannot provide.
Ultimately, the teach of following your Basal Body Temperature is an act of strengthening. It changes unique real forms into substantial, interpretable information, preparing ladies with significant information around their regenerative wellbeing and cultivating more educated discussions with healthcare suppliers.